Welcome the to the County of San Diego Behavioral Health Plan Credentialing and Enrollment page for Organizational Providers
If you are a provider, please select Provider from the options below in order to access all of the information and documents you will need to complete your credentialing and potential enrollment. If you are a legal entity or program representative, please select Entity/Program from the options below in order to access all of the requirements for entities which are participating in the System of Care and their responsibilities to their providers.
- If you are part of or trying to join the TERM network then please click here to be taken to the correct page.
- If you are part of or trying to join the Fee For Service network then please click here to be taken to the correct page.
Provider Requirements
Credentialing Requirement for Organizational Providers
This credentialing process is mandated by the State and is not optional. Further details over requirements mandated by the Department of Healthcare Services regarding credentialing can be found here.
After initial credentialing, recredentialing will be required every 3 years to maintain your participation in the network.
You are required to undergo and complete the credentialing process within your first month of employment if all the following apply to you:
- You are employed by a Program or are a facility that is serving Medi-Cal clients/funded by Medi-Cal
- You render direct services to patients
- If you are an individual provider, you have one of the following disciplines listed below:
- Associate Marriage Family Therapist
- Associate Professional Clinical Counselor
- Associate Clinical Social Worker
- Doctor of Medicine
- Doctor of Osteopathic Medicine
- Licensed Clinical Social Worker
- Licensed Marriage Family Therapist
- Licensed Professional Clinical Counselor
- Licensed Psychiatric Technician
- Licensed Vocational Nurse
- Nurse Practitioner
- PhD Licensed
- PhD Registered
- Psych Assistant
- PsyD Licensed
- PsyD Registered
- Registered Nurse
- Waivered - PhD / PsyD
- SUD Counselor- Certified: This discipline applies to providers that have earned a certification from any of the following organizations:
- CCAPP
- CADTP
- CAADE
- SUD Counselor – Registered: This discipline applies to providers that have registered with any of the following organizations:
- CCAPP
- CADTP
- CAADE
Enrollment Requirement for Organizational Providers
To ensure compliance with the Cures Act and Final Rule mandates, DHCS is requiring that
MHPs ensure all applicable network providers, including individual rendering providers and
SMH facilities, enroll through DHCS’ Provider Application and Validation for Enrollment
(PAVE) portal (unless the facility is required to enroll via CPDH). Additional enrollment requirements can be found here.
You are required to undergo and complete the enrollment process within 120 days of your hire date, if all the following apply to you:
- You are employed by a Program or are a Facility that is serving Medi-Cal clients/funded by Medi-Cal
- You render direct services to patients
- If you are an individual provider, you have one of the following disciplines listed below:
- Doctor of Medicine
- Doctor of Osteopathic Medicine
- Licensed Clinical Social Worker
- Licensed Marriage Family Therapist
- Licensed Professional Clinical Counselor
- Nurse Practitioner
- PhD Licensed
- Physician’s Assistant
- PsyD Licensed
Process Timelines
Initial Credentialing
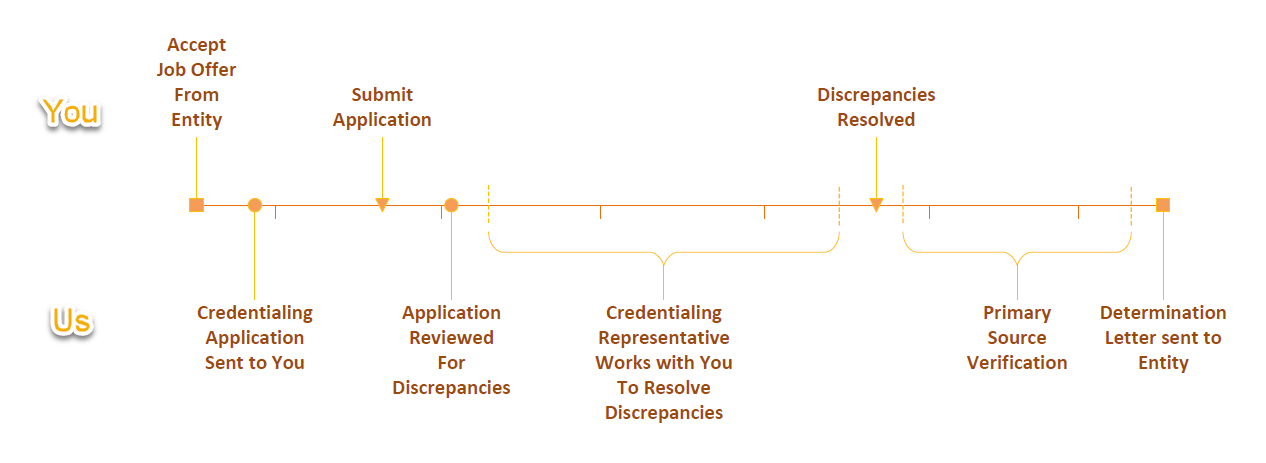
Upon your acceptance of an offer of employment, your entity will send a notice to Optum with your information to get your credentialing process started. Your assigned Optum Credentialing Representative will prepare and send the credentialing application to you electronically. IMPORTANT: Applications are time sensitive and must be completed as soon as possible as you will only be able to start providing services and bill once credentialing and other applicable requirements are completed. Upon submitting your completed and signed application, your Optum Credentialing Representative will review it to ensure that it is complete and work with you to correct any discrepancies. Once your application is complete and free of discrepancies, we will begin to Primary Source Verify the information and documents submitted. This process typically takes about two to three weeks. Once the review is complete, a determination letter is sent to your employer.
Enrollment

Upon initiating the credentialing process or upon notification of a change in discipline, the Enrollment Coordinator will verify your need for enrollment. If enrollment is required, an application will be prepared on your behalf. Once the application is prepared, an invitation to join PAVE is sent to you electronically. You are requested to join PAVE to review, attest, and sign your enrollment application within 5 business days of receiving your invitation. IMPORTANT: Do not submit the application. Send a reply to the Enrollment Coordinator and they will verify and submit the application to DHCS’ Provider Enrollment Division (PED). Once submitted, the PED review process may take up to 90 days for physicians, and 180 days for non-physicians. Once the review is complete, the determination letter will be sent to your employer.
Recredentialing
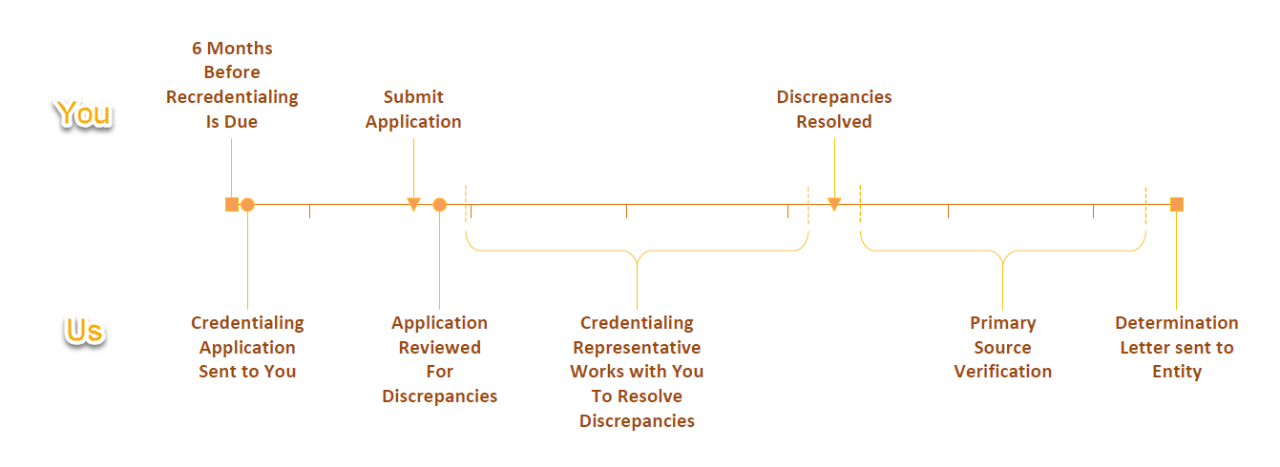
After your initial credentialing has been approved, recredentialing will be required every three years to maintain your participation in the network. Six months before the three-year mark, your assigned Optum Credentialing Representative will reach out and provide you with the recredentialing application. The rest of the timeline for this process is the same as Initial Credentialing.
Applications Process
Credentialing
Preparation for Your Application
NPPES NPI
You will be required to have an NPI to participate in the network. If you are unsure of your NPI, you can look it up here: NPPES NPI Registry
If you do not have an NPI, you can obtain one here: NPPES
You will be asked to provide this number on the application, so it is recommended that you look it up or obtain it before you receive your application to minimize delays.
Required Documents
While filling out your credentialing application, you will need to supply copies/pictures of various documents. To make the process as smooth as possible for yourself, please make these copies or snap the pictures before you receive your application so that you can have them ready to attach and upload once you receive it.
Three documents which you will have to supply are:
- Any license/registration/certification which qualifies you for your position
- Your California Driver License or State ID
- Your up-to-date CV/Resume, which lists all paid employment held in the last 5 years.
The most common delay in the credentialing process is a resume which is out of date or is missing paid positions you held in the last 5 years, so please make sure yours is good to go.
Filling Out Your Application
Your application will be sent electronically via Adobe Sign to your professional email address provided by your employer. The email will contain a link to access the application. Please do not use a mobile device to access the application since that may cause errors and prevent you from being able to submit the application. When you click on the link in the email, it will open the application in your web browser.
You only need to fill in the required fields which are highlighted with a red asterisk.
If you need help filling out your application, we have two valuable resources for you. One is online help. It is available 24/7 under the Applications section of this site. Just click the Applications button to be taken there. The online help provides detailed step by step instructions and tutorial videos for each section of the application. If you still have questions that aren’t answered there, you are also welcomed to reach out to your assigned Optum Credentialing Representative. They are available Monday – Friday during their regular office hours. If you don’t have an assigned representative yet, you can send your questions to BHSCredentialing@optum.com or call us at 800-482-7114 and one of us would be more than happy to assist.
Submitting Your Application
After all required fields have been filled and the application has been signed, you will be able to submit it via Adobe Sign. A copy of the completed application will be sent to you, us, and your entity’s credentialing contact.
Enrollment
To initiate enrollment, there are no additional steps you must take other than completing the credentialing process. We strive to align credentialing and enrollment as parallel processes to ensure timeliness. When you return a credentialing application, Optum’s Enrollment Coordinator will be notified and will review if you require enrollment. If you require enrollment, the Enrollment Coordinator will prepare an application on your behalf, utilizing the information collected during credentialing.
Preparation for Your Application
Required Documents
During the enrollment process, the Enrollment Coordinator will work with your Credentialing Representative to collect the required documents. If the documents required are invalid or expired, the Credentialing Representative will request updated documentation from you.
The documents which you may have to supply are:
- A legible copy of your current professional license issued by the appropriate licensing agency.
- A legible copy of your current pocket license or the original diploma-style wall certificate may also be accepted. DHCS will not accept website confirmation as proof of licensure.
- A legible copy of your current State-Issued Driver License or Identification Card.
Filling Out Your Application
Once your application is ready, you will receive a PAVE invitation electronically. The invitation will include a link to DHCS’ Medi-Cal website, the PAVE Provider Portal. Once you have created your PAVE account and accepted access, the application will be visible under the applications tab of your profile. Please review the application for updates, if necessary. As the Enrollment Coordinator cannot attest or sign on your behalf, you will be required to complete the application’s disclosure information and signature sections.
If you require assistance throughout the enrollment process, there are several resources on hand. You will receive instructions via email which include an enrollment guidance pdf providing step by step instructions with visual aids. If you have any questions or concerns, please do not hesitate to reach out to the Enrollment Coordinator, Sarahi Alcaraz, via phone or email. She is available Monday-Friday, during her regular office hours.
Submitting Your Application
IMPORTANT: Please do not submit your application within the PAVE Portal. Once you have completed the disclosure information and signature sections and the application reflects 96% completion, you should close out of PAVE. Once this is done, please send an email to the Enrollment Coordinator and we will finalize the submission.
Recredentialing
Six (6) months before your recredentialing due date, your assigned Optum Credentialing Representative will reach out to you and provide the Recredentialing Application via Adobe Sign.
Preparation for Your Application
Required Documents
For the recredentialing process, you may have to submit your most up to date valid and unexpired documents if the previous copies expired in the interim 3 years. The two documents which you may have to supply are:
- Any license/registration/certification which qualifies you for your position if the previous one expired.
- Your California Driver License or State ID if the previous one expired.
- Depending on your discipline, you may have to resubmit previously submitted documents if they have expired.
- Written statements for any “Yes” answers to attestation questions.
Filling Out Your Application
Your application will be sent electronically via Adobe Sign to your professional email address provided by your employer. The email will contain a link to access the application. Please do not use a mobile device to access the application since that may cause errors and prevent you from being able to submit the application. When you click on the link in the email, it will open the application in your web browser.
The application you receive will be prefilled with the information from your previous application where possible. For those prefilled areas, all you must do is confirm that the information is correct or make any changes necessary.
If you need help filling out your application, we have two valuable resources for you. One is online help. It is available 24/7 under the Applications section of this site. Just click the Applications button to be taken there. The online help provides detailed step by step instructions and tutorial videos for each section of the application. If you still have questions that aren’t answered there, you are also welcomed to reach out to your assigned Optum Credentialing Representative. They are available Monday – Friday during their regular office hours. If you don’t have an assigned representative yet, you can send your questions to BHSCredentialing@optum.com or call us at 800-482-7114 and one of us would be more than happy to assist.
Submitting Your Application
Once you have updated or confirmed all the info and attached the requested documents, you will be able to submit it via Adobe Sign. A copy of the completed application will be sent to you, us, and your entity’s credentialing contact.
Entity & Program Requirements
Credentialing Requirement for Organizational Providers
Upon acceptance of employment offer for a new hire, you must send a notice to Optum with the provider's information (new hire info) to get their credentialing process started. The assigned Optum Credentialing Representative will prepare and send the credentialing application to the provider via email within a business day of the notice. Once the provider has received their application, they will have 30 days to complete and submit it. After they have submitted their application, the Optum Credentialing Representative will review it to ensure that it is complete and work with the provider to correct any discrepancies. Once the application is complete and free of discrepancies, we will begin to Primary Source Verify the information and documents submitted. This process typically takes about two to three weeks. Once it is complete, if any discrepancies are found, the provider will be sent a formal notice and given a chance to address the discrepancies before the application is sent to our medical review board. Once the review is complete, a determination letter is sent to your entity explaining whether the provider can participate in the network.
Disciplines Requiring Credentialing:
- Associate Marriage Family Therapist
- Associate Professional Clinical Counselor
- Associate Clinical Social Worker
- Doctor of Medicine
- Doctor of Osteopathic Medicine
- Licensed Clinical Social Worker
- Licensed Marriage Family Therapist
- Licensed Professional Clinical Counselor
- Licensed Psychiatric Technician
- Licensed Vocational Nurse
- Nurse Practitioner
- PhD Licensed
- PhD Registered
- Psych Assistant
- PsyD Licensed
- PsyD Registered
- Registered Nurse
- Waivered - PhD / PsyD
- SUD Counselor- Certified: This discipline applies to providers that have earned a certification from any of the following organizations:
- CCAPP
- CADTP
- CAADE
- SUD Counselor – Registered: This discipline applies to providers that have registered with any of the following organizations:
- CCAPP
- CADTP
- CAADE
- All Others: If you are unsure if a discipline or taxonomy is required to undergo the credentialing process, please send an email to BHSCredentialing@optum.com to find out.
Enrollment Requirement for Organizational Providers
To ensure compliance with the Cures Act and Final Rule mandates, DHCS is requiring that
MHPs ensure all applicable network providers, including individual rendering providers and
SMH facilities, enroll through DHCS' Provider Application and Validation for Enrollment
(PAVE) portal (unless the facility is required to enroll via CPDH). Additional enrollment requirements can be found here.
Providers you hire are required to undergo and complete the enrollment process within 120 days of their hire date, if all the following apply to them:
- They are employed by a Program or are a facility that is serving Medi-Cal clients/funded by Medi-Cal
- They render direct services to patients
- If they are an individual provider, they have one of the following disciplines listed below:
- Doctor of Medicine
- Doctor of Osteopathic Medicine
- Licensed Clinical Social Worker
- Licensed Marriage Family Therapist
- Licensed Professional Clinical Counselor
- Nurse Practitioner
- PhD Licensed
- Physician's Assistant
- PsyD Licensed
Process Timelines
Initial Credentialing
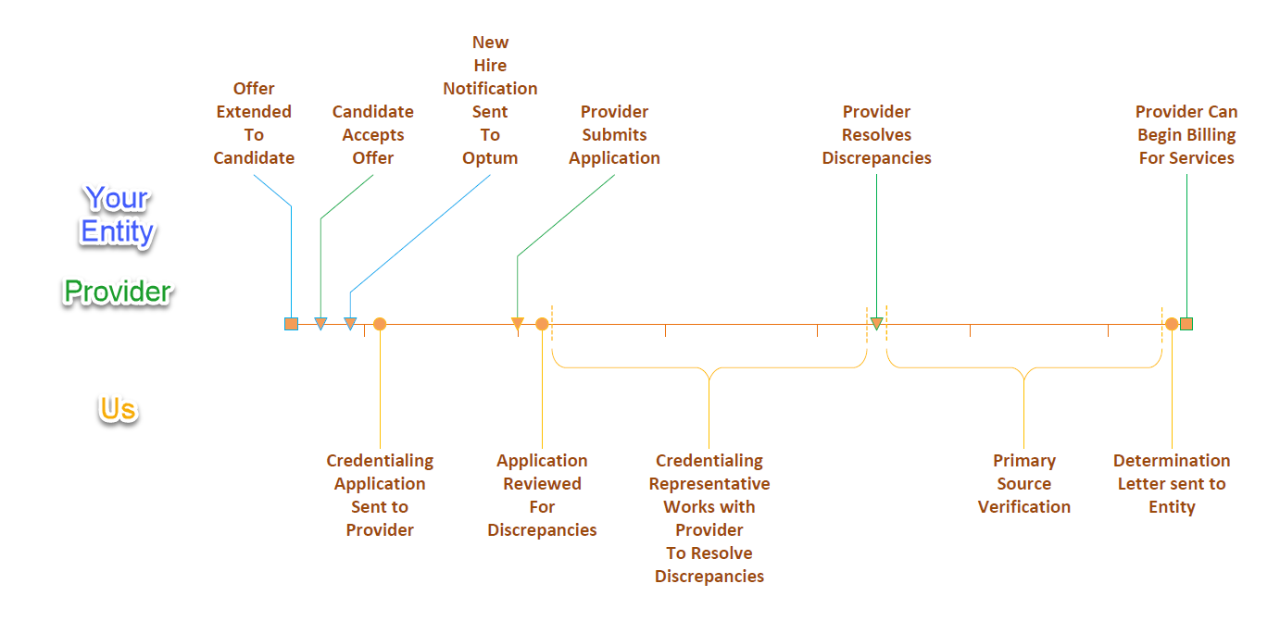
Upon acceptance of employment offer for a new hire, you must send a notice to Optum with the provider’s information (new hire info) to get their credentialing process started. The assigned Optum Credentialing Representative will prepare and send the credentialing application to the provider via email within a business day of the notice. Once the provider has received their application, they will have 30 days to complete and submit it. After they have submitted their application, the Optum Credentialing Representative will review it to ensure that it is complete and work with the provider to correct any discrepancies. Once the application is complete and free of discrepancies, we will begin to Primary Source Verify the information and documents submitted. This process typically takes about two to three weeks. Once it is complete, if any discrepancies are found, the provider will be sent a formal notice and given a chance to address the discrepancies before the application is sent to our medical review board. Once the review is complete, a determination letter is sent to your entity explaining whether the provider can participate in the network.
Enrollment
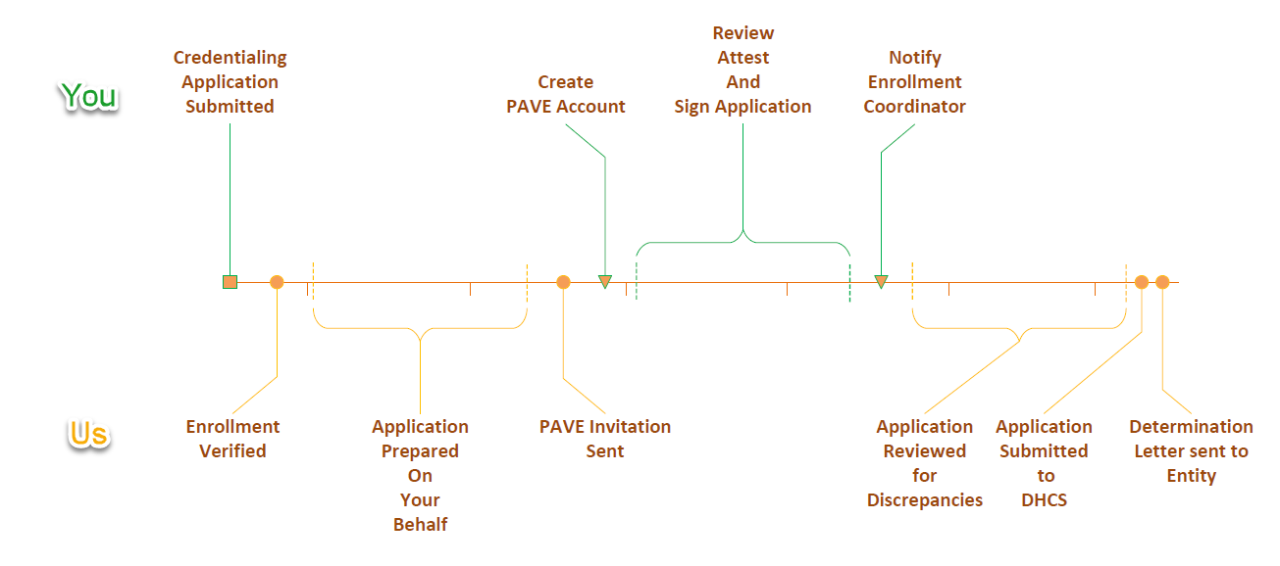
Upon initiating the credentialing process or upon notification of a change in discipline, the Enrollment Coordinator will verify the provider's need for enrollment. If enrollment is required, an application will be prepared on their behalf. Once the application is prepared, an invitation to join PAVE is sent to the provider electronically. The provider will join PAVE to review, attest, and sign their enrollment application within 5 business days of receiving their invitation. IMPORTANT: Providers must not submit the application. The provider will send a reply to the Enrollment Coordinator who will finalize submission to DHCS' Provider Enrollment Division (PED). Once submitted, the PED review process may take up to 90 days for physicians, and 180 days for non-physicians. Once the review is complete, the determination letter will be sent to you.
Recredentialing
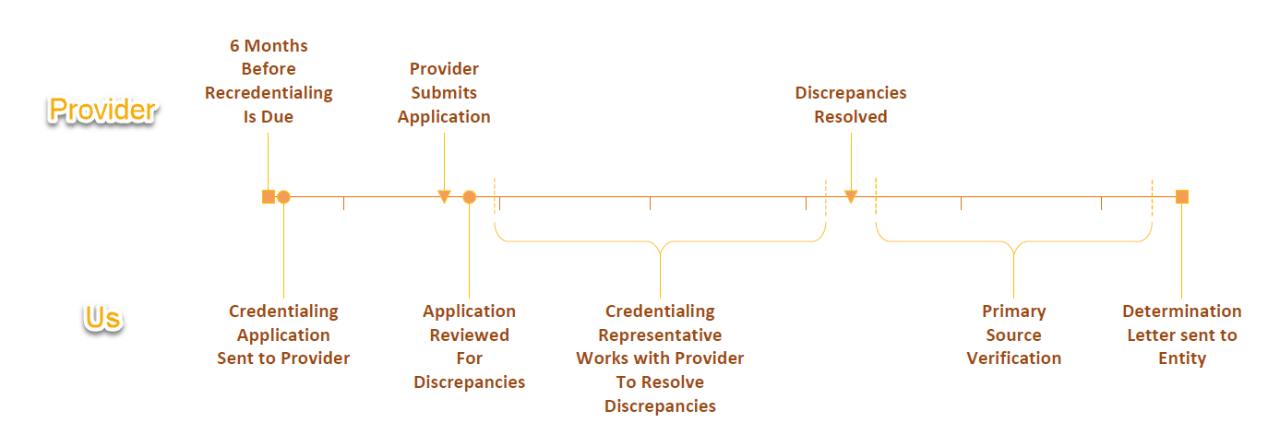
After a provider's initial credentialing has been approved, recredentialing will be required every three years. Six months before the three-year mark, the assigned Optum Credentialing Representative will reach out to the provider and provide them with the recredentialing application. The rest of the timeline for this process is the same as Initial Credentialing.
Application Process
Credentialing
Preparation for the Application
NPPES NPI
Providers are required to have an NPI number to participate in the network. You are also asked to provide this NPI whenever you send a New Hire notification as detailed in this section. If you are unsure of a provider's NPI, you can look it up here: NPPES NPI Registry
If a provider does not have an NPI, they can obtain one here: NPPES
Providers will be asked to provide this number on their credentialing application, so it is recommended that they look it up or obtain it before they receive their application to minimize delays.
Required Documents
While filling out the credentialing application, a provider will need to supply copies/pictures of various documents. To make the process as smooth as possible for the provider, please remind them to make these copies or snap the pictures upon hire, before they receive their application, so that they can have them ready to attach and upload once they receive the application.
Three documents which a provider will have to supply are:
- Any license/registration/certification which qualifies them for their position
- Their California Driver License or State ID
- Their up-to-date CV/Resume, which lists all paid employment held in the last 5 years.
The most common delay in the credentialing process is a resume which is out of date or is missing paid positions they held in the last 5 years, so please make sure your providers understand this and update their resume accordingly.
Filling Out the Application
The application will be sent electronically via Adobe Sign to the provider's professional email address provided by your entity. The email will contain a link to access the application. Please remind providers not to use a mobile device to access the application since that may cause errors and prevent them from being able to submit the application. When they click on that link, it will open the application in their web browser.
They will only need to fill in the required fields. They can skip the other fields if they don't have the information.
If providers need help filling out their application, we have two valuable resources for them. One is online help. It is available 24/7 under the Applications section of this site. It can be accessed by clicking the Applications button. The online help provides detailed step by step instructions and tutorial videos for each section of the application. If they still have questions that aren't answered there, they are welcome to reach out to their assigned Optum Credentialing Representative. Our representatives are available Monday – Friday during their regular office hours. If a provider doesn't have an assigned representative yet, they can send their questions to BHSCredentialing@optum.com and one of us would be more than happy to assist.
Submitting the Application
After all required fields have been filled and the application has been signed, providers will be able to submit it via Adobe Sign. A copy of the completed application will be sent to the provider, us, and possibly your entity's credentialing contact.
Enrollment
To initiate enrollment, there are no additional steps a provider must take other than completing the credentialing process. We strive to align credentialing and enrollment as parallel processes to ensure timeliness. When a provider returns a credentialing application, Optum's Enrollment Coordinator will be notified and will review if the provider requires enrollment. If the provider requires enrollment, the Enrollment Coordinator will prepare an application on their behalf, utilizing the information collected during credentialing.
Preparation for the Application
Required Documents
During the enrollment process, the Enrollment Coordinator will work with the provider's Credentialing Representative to collect the required documents for their application. If the documents on file are invalid or expired, the Credentialing Representative will request updated documentation from the Provider.
The documents which the provider or credentialing contact may have to supply are:
- A legible copy of the provider's current professional license issued by the appropriate licensing agency.
- A legible copy of their current pocket license or the original diploma-style wall certificate may also be accepted. DHCS will not accept website confirmation as proof of licensure.
- A legible copy of the provider's current State-Issued Driver License or Identification Card.
Filling Out the Application
Once the application is ready, the provider will receive a PAVE invitation electronically. The invitation will include a link to DHCS' Medi-Cal website, the PAVE Provider Portal. Once the provider has created a PAVE account and accepted access, the application will be visible under the applications tab of their profile. They should review the application for updates, if necessary. As the Enrollment Coordinator cannot attest or sign on the provider's behalf, they will be required to complete the application's disclosure information and signature sections.
If they require assistance throughout the enrollment process, there are several resources on hand. They will receive instructions via email which include an enrollment guidance pdf providing step by step instructions with visual aids. If they have any questions or concerns, they are welcome to reach out to the Enrollment Coordinator, Sarahi Alcaraz, via phone or email. She is available Monday-Friday, during her regular office hours.
Submitting the Application
IMPORTANT: Please ensure providers do not submit their application within the PAVE Portal. Once they have completed the disclosure information and signature sections and the application reflects 96% completion, they should close out of PAVE. Once this is done, they should send an email to the Enrollment Coordinator and we will finalize the submission.
Recredentialing
Six (6) months before a provider's recredentialing due date, their assigned Optum Credentialing Representative will reach out to them and provide the Recredentialing Application via Adobe Sign.
Preparation for the Application
Required Documents
For the recredentialing process, a provider may have to submit their most up to date valid and unexpired documents if the previous copies expired in the interim 3 years. The documents which a provider may have to supply are:
- Any license/registration/certification which qualifies them for their position, if the previous one expired.
- Their California Driver License or State ID if the previous one expired.
- Depending on their discipline, they may have to resubmit previously submitted documents if they have expired.
- Written statements for any “Yes” answers to attestation questions.
Filling Out the Application
Their application will be sent electronically via Adobe Sign to their professional email address provided by your entity. The email will contain a link to access the application. Please ensure providers do not use a mobile device to access the application since that may cause errors and prevent them from being able to submit the application. When they click on the link in the email, it will open the application in their web browser.
The application they receive will be prefilled with the information from their previous application where possible. For those prefilled areas, all they must do is confirm that the information is correct or make any changes necessary.
If they need help filling out their application, we have two valuable resources for them. One is online help. It is available 24/7 under the Applications section of this site. Just click the Applications button to be taken there. The online help provides detailed step by step instructions and tutorial videos for each section of the application. If they still have questions that aren't answered there, they are also welcomed to reach out to their assigned Optum Credentialing Representative. Representatives are available Monday – Friday during their regular office hours. If they don't have an assigned representative yet, they can send their questions to BHSCredentialing@optum.com or call us at 800-482-7114 and one of us would be more than happy to assist.
Submitting the Application
Once they have updated or confirmed all the info and attached the requested documents, they will be able to submit it via Adobe Sign. A copy of the completed application will be sent to them, us, and your entity's credentialing contact.
Responsibility to Providers
Legal Entities which are contracted with the County of San Diego to provide services for System of Care patients and employ organizational providers, have certain responsibilities regarding their providers.
Entities must make sure to submit new hire notifications to Optum upon a new provider accepting a job offer. Delays in sending the notification can lead to a provider being unable to provide services until credentialing is complete. See the section titled New Hire Notifications for more details.
Entities are responsible to ensure that their providers complete the credentialing application within 30 days of it being sent. Delays in submitting the application in the time frame allotted can lead to a provider being unable to provide services until credentialing is complete.
New Hire Notifications
Any time that your entity hires an organizational provider that has one of the disciplines listed below and will be providing services directly to patients, you must make sure to send a new hire notification to us as soon as the offer of employment is accepted by the provider. This helps us complete the provider’s credentialing process before they begin to bill for services.
Disciplines requiring a new hire notification:
- Associate Marriage Family Therapist
- Associate Professional Clinical Counselor
- Associate Clinical Social Worker
- Doctor of Medicine
- Doctor of Osteopathic Medicine
- Licensed Clinical Social Worker
- Licensed Marriage Family Therapist
- Licensed Professional Clinical Counselor
- Licensed Psychiatric Technician
- Licensed Vocational Nurse
- Nurse Practitioner
- PhD Licensed
- PhD Registered
- Psych Assistant
- PsyD Licensed
- PsyD Registered
- Registered Nurse
- Waivered - PhD / PsyD
- SUD Counselor- Certified: This discipline applies to providers that have earned a certification from any of the following organizations:
- CCAPP
- CADTP
- CAADE
- SUD Counselor – Registered: This discipline applies to providers that have registered with any of the following organizations:
- CCAPP
- CADTP
- CAADE
- All Others: If you are unsure if a discipline or taxonomy requires a new hire notification, please send an email to BHSCredentialing@optum.com to find out.
Send the following information in an email to BHSCredentialing@optum.com to notify us of a new hire:
- Provider’s Name
- Provider’s NPI (Required – see Application Processes for details on obtaining correct NPI)
- Provider’s Email Address
- Date of hire
- Provider’s discipline from the list above
- Name of program they will be working for
- Program Manager

